Decoding Lupus Diagnosis: A Guide To Identifying This Complex Condition
Lupus, a chronic autoimmune disease, often presents a perplexing challenge in the realm of medical diagnostics. Known for its ability to mimic other diseases and manifest with a wide array of symptoms, lupus diagnosis requires a meticulous approach. From its unpredictable flare-ups to its impact on various body systems, the journey to accurately diagnosing lupus can be fraught with hurdles. For patients and healthcare providers alike, understanding the intricacies of lupus diagnosis is crucial for effective management and treatment.
In the world of healthcare, lupus stands as a medical enigma. Its symptoms can vary drastically from one person to another, with manifestations that include joint pain, skin rashes, and fatigue. The complexity of lupus diagnosis is further compounded by the fact that these symptoms can overlap with those of other conditions, leading to potential misdiagnosis or delayed treatment. This article delves into the essential aspects of lupus diagnosis, shedding light on the techniques and criteria used by medical professionals to pinpoint this elusive disease.
As we explore lupus diagnosis, we'll uncover the significance of early detection and the vital role of patient education. With advancements in medical research and technology, the process of diagnosing lupus has become more refined, yet it remains a field that demands ongoing attention and expertise. Through this comprehensive guide, we aim to equip readers with a deeper understanding of lupus diagnosis, empowering them to navigate the complexities of this condition with confidence and clarity.
Read also:Palantir Technologies Transforming The Future Of Data Analytics And Decisionmaking
Table of Contents
- What is Lupus?
- How Does Lupus Affect the Body?
- Common Symptoms of Lupus
- Why is Lupus Diagnosis Challenging?
- The Role of Medical History in Lupus Diagnosis
- Physical Examinations and Lupus Diagnosis
- Laboratory Tests Used in Lupus Diagnosis
- What are ANA Tests and Their Significance?
- Imaging Tests in the Diagnosis of Lupus
- Criteria for Lupus Diagnosis
- Differential Diagnosis: Why it Matters?
- Impact of Delayed Lupus Diagnosis
- Treatment Options After Lupus Diagnosis
- Living with Lupus: Managing the Condition
- Future Prospects in Lupus Diagnosis
What is Lupus?
Lupus is an autoimmune disease where the body's immune system becomes hyperactive and attacks normal, healthy tissue. This behavior causes inflammation, swelling, and damage to joints, skin, kidneys, blood, heart, and lungs. The most common form of lupus is systemic lupus erythematosus (SLE), which affects multiple organs. Its exact cause remains unknown, but it is believed to result from a combination of genetic, environmental, and hormonal factors.
Autoimmunity is the hallmark of lupus, where the immune system fails to distinguish between foreign invaders and the body's own cells. This misidentification leads to the production of antibodies that target the body's tissues, causing widespread symptoms. The onset of lupus can occur at any age, though it most commonly appears between the ages of 15 and 45. Women, particularly those of African, Asian, or Hispanic descent, are at a higher risk of developing lupus.
The diversity in symptoms and the unpredictable nature of lupus make it a particularly challenging condition to diagnose. Patients may experience periods of remissions and flares, where symptoms temporarily improve only to worsen later. This cyclical pattern underscores the importance of understanding the full spectrum of lupus to achieve an accurate diagnosis and effective management plan.
How Does Lupus Affect the Body?
Lupus can impact nearly every part of the body, with symptoms that range from mild to severe. The inflammation caused by lupus can lead to damage in various organs and systems, manifesting in diverse ways. Understanding how lupus affects different body parts is crucial for recognizing its signs and seeking timely medical intervention.
One of the most commonly affected areas is the skin, where lupus can cause rashes and lesions. The classic butterfly-shaped rash across the cheeks and nose is a hallmark of the disease. Additionally, lupus can lead to photosensitivity, where exposure to sunlight exacerbates skin issues.
Joint pain and swelling are also prevalent in lupus patients, often mimicking arthritis. Lupus can cause stiffness, tenderness, and swelling in the joints, particularly in the mornings. Over time, this can lead to more significant mobility issues if not properly managed.
Read also:Gary Watson Garden Gner Your Guide To A Flourishing Landscape
The kidneys are another critical area affected by lupus. Lupus nephritis, an inflammation of the kidneys, can lead to serious complications such as kidney failure if left untreated. Symptoms may include swelling in the legs and feet, high blood pressure, and foamy urine due to protein leakage.
Lupus can also impact the cardiovascular system, increasing the risk of heart disease. Inflammation of the heart muscle, arteries, or heart membrane (pericarditis) can occur, leading to chest pain and other cardiovascular issues. The disease can also affect the lungs, causing pleuritis (inflammation of the lung lining) and increasing the risk of pneumonia.
The nervous system is not immune to the effects of lupus. Patients may experience headaches, dizziness, memory issues, and even seizures or strokes. These neurological symptoms can be particularly challenging to manage and may require specialized care.
Given the widespread impact of lupus on the body, a comprehensive understanding of its potential effects is essential for both patients and healthcare providers. This knowledge can guide the diagnostic process and inform treatment strategies, ultimately improving patient outcomes.
Common Symptoms of Lupus
Lupus is notorious for its wide range of symptoms, which can affect different parts of the body. Recognizing these symptoms is a vital step in the diagnostic process. While each patient may experience lupus differently, some common symptoms are frequently observed.
- Fatigue: A profound and chronic sense of tiredness that is not alleviated by rest.
- Joint pain and swelling: Often affecting the wrists, knees, and fingers.
- Skin rashes: Including the characteristic butterfly rash across the nose and cheeks.
- Fever: Unexplained fevers without infection.
- Hair loss: Thinning hair or hair loss in patches.
- Photosensitivity: Sensitivity to sunlight, causing rashes or exacerbating other symptoms.
- Raynaud's phenomenon: Color changes in the fingers and toes in response to cold or stress.
- Chest pain: Often caused by pleuritis or pericarditis.
- Kidney issues: Manifesting as swelling in the legs and feet or foamy urine.
- Neurological symptoms: Including headaches, dizziness, and memory problems.
These symptoms can vary in severity and may come and go, complicating the diagnosis. Some patients may only experience mild symptoms, while others face severe and life-threatening complications. The variability and overlap of symptoms with other conditions highlight the importance of a thorough and careful assessment by healthcare professionals.
Why is Lupus Diagnosis Challenging?
Lupus diagnosis is notoriously challenging due to the disease's complex nature and the wide range of symptoms that can mimic other conditions. This complexity requires a multifaceted approach to accurately identify and diagnose the disease.
One significant challenge in lupus diagnosis is the variability of symptoms. Patients can present with different symptoms at different times, making it difficult to establish a consistent pattern. Additionally, these symptoms often overlap with those of other autoimmune diseases, such as rheumatoid arthritis or fibromyalgia, leading to potential misdiagnosis.
The lack of a single definitive test for lupus adds another layer of difficulty. Instead, doctors rely on a combination of laboratory tests, clinical evaluations, and patient history to make a diagnosis. This process can be time-consuming and may require multiple visits and tests to reach a conclusive diagnosis.
Furthermore, lupus can affect multiple organs, and its symptoms can evolve over time, complicating the diagnostic process. Some patients may not meet the full criteria for lupus initially, but their symptoms may progress to fulfill the diagnostic criteria later.
Healthcare providers must also consider the potential for false positives or negatives in laboratory tests. For example, a positive antinuclear antibody (ANA) test is common in lupus patients, but it can also occur in healthy individuals or those with other conditions.
The challenge of diagnosing lupus underscores the importance of experienced healthcare providers who can navigate the complexity of the disease. A thorough understanding of lupus, combined with careful clinical evaluation and appropriate use of diagnostic tools, is essential for accurate diagnosis and effective management.
The Role of Medical History in Lupus Diagnosis
A detailed medical history is a cornerstone in the lupus diagnosis process. Understanding a patient's past health experiences, family history, and symptom development can provide valuable insights into the potential presence of lupus.
During a medical history assessment, healthcare providers will inquire about various aspects of the patient's health, including:
- Onset and progression of symptoms: Documenting when symptoms first appeared and how they have changed over time.
- Family history: Identifying any relatives with autoimmune diseases or similar symptoms.
- Previous medical conditions: Reviewing past diagnoses and treatments to identify potential patterns or connections.
- Medications and allergies: Examining any current or past medications that could influence symptoms or test results.
- Lifestyle factors: Considering environmental exposures, diet, and stress levels that could impact health.
This comprehensive history helps healthcare providers piece together a holistic view of the patient's health, guiding the diagnostic process. It also allows them to rule out or consider other conditions that may present with similar symptoms.
The accuracy and detail of the medical history can significantly influence the diagnostic outcome. Patients are encouraged to be thorough and honest in their responses, as even seemingly unrelated information can be critical in identifying lupus.
Physical Examinations and Lupus Diagnosis
Physical examinations play a crucial role in the lupus diagnosis process, allowing healthcare providers to assess the physical manifestations of the disease. These examinations can provide direct evidence of lupus-related symptoms and help guide further diagnostic testing.
During a physical examination for lupus, healthcare providers will typically evaluate the following:
- Skin: Checking for rashes, lesions, and photosensitivity reactions.
- Joints: Assessing for swelling, tenderness, and range of motion.
- Lymph nodes: Palpating for any enlargement or tenderness.
- Heart and lungs: Listening for abnormal sounds, such as murmurs or friction rubs.
- Abdomen: Checking for organ enlargement or tenderness.
- Nervous system: Evaluating reflexes, coordination, and mental status.
The findings from a physical examination can provide valuable clues about the presence and extent of lupus. They can also help determine which additional tests or referrals may be necessary for a more comprehensive evaluation.
In some cases, healthcare providers may use specialized tools, such as a dermatoscope, to examine skin lesions more closely. This level of detail can aid in distinguishing lupus rashes from other skin conditions.
Physical examinations are a critical component of lupus diagnosis, offering direct insights into the disease's impact on the body. When combined with medical history and laboratory testing, they help form a complete picture of the patient's health and guide the diagnostic process.
Laboratory Tests Used in Lupus Diagnosis
Laboratory tests are a vital part of the lupus diagnosis process, providing objective data that can help confirm or rule out the disease. While no single test can definitively diagnose lupus, a combination of tests can offer valuable insights into the presence and activity of the disease.
Some of the key laboratory tests used in lupus diagnosis include:
- Antinuclear Antibody (ANA) Test: A positive ANA test is common in lupus patients and is often the first test ordered when lupus is suspected. However, a positive result alone is not sufficient for diagnosis, as it can also occur in healthy individuals or those with other conditions.
- Anti-DNA and Anti-Smith Antibodies: These antibodies are more specific to lupus and can help confirm the diagnosis when present.
- Complement Levels: Low levels of complement proteins (C3 and C4) may indicate active lupus, as they are consumed during the inflammatory process.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These tests measure inflammation in the body and can indicate disease activity.
- Complete Blood Count (CBC): This test can reveal anemia, low white blood cell count, or low platelet count, which are common in lupus patients.
- Urinalysis: Assessing kidney function by detecting protein or blood in the urine, which may suggest lupus nephritis.
The interpretation of these tests requires expertise, as results can vary based on individual factors and the presence of other conditions. Healthcare providers must consider the entire clinical picture, integrating laboratory data with clinical findings and medical history.
Laboratory tests are an essential tool in the lupus diagnosis process, offering quantifiable evidence that can support clinical observations. When used in conjunction with other diagnostic methods, they can help healthcare providers make informed decisions about the presence and management of lupus.
What are ANA Tests and Their Significance?
The Antinuclear Antibody (ANA) test is a crucial component in the lupus diagnosis process, serving as a primary screening tool for autoimmune diseases. ANAs are antibodies that target structures within the nucleus of cells, and their presence can indicate an autoimmune response.
In the context of lupus diagnosis, a positive ANA test is often one of the first indicators that prompts further investigation. While a positive result is common in lupus patients, it is not exclusive to the disease. A positive ANA test can also occur in healthy individuals, those with other autoimmune diseases, or even due to certain medications.
Despite this, the ANA test remains a valuable tool in the diagnostic process. It helps identify patients who may require further testing for more specific antibodies associated with lupus, such as anti-DNA or anti-Smith antibodies.
The significance of the ANA test lies in its ability to guide the diagnostic process and provide a starting point for further evaluation. Healthcare providers must interpret the results within the context of the patient's symptoms, medical history, and other test results to make an accurate diagnosis.
While the ANA test is not definitive for lupus, it is an essential part of the diagnostic toolkit, providing valuable information that can help healthcare providers identify potential autoimmune activity and guide further testing.
Imaging Tests in the Diagnosis of Lupus
Imaging tests can play a supportive role in the lupus diagnosis process, providing visual evidence of the disease's impact on internal organs and structures. While not typically used as a primary diagnostic tool, imaging tests can offer valuable insights into the extent and severity of lupus-related damage.
Some of the imaging tests that may be used in the diagnosis of lupus include:
- Ultrasound: This non-invasive test can assess joint inflammation and detect fluid accumulation in the joints or organs, such as the kidneys.
- X-rays: Used to evaluate joint damage or inflammation in cases where arthritis-like symptoms are present.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the brain and spinal cord, useful for assessing neurological symptoms or complications.
- Computed Tomography (CT) Scan: Offers cross-sectional images of the body, helpful in evaluating lung involvement or other internal organ issues.
- Echocardiogram: Assesses heart function and can detect inflammation of the heart membrane (pericarditis) or other cardiac issues.
The choice of imaging tests depends on the specific symptoms and suspected areas of involvement. These tests can help healthcare providers visualize the internal effects of lupus and guide treatment decisions based on the severity of organ damage.
While imaging tests are not definitive for diagnosing lupus, they provide complementary information that can enhance the overall understanding of the disease's impact on the body. When used in conjunction with clinical evaluations and laboratory tests, imaging studies contribute to a comprehensive approach to lupus diagnosis and management.
Criteria for Lupus Diagnosis
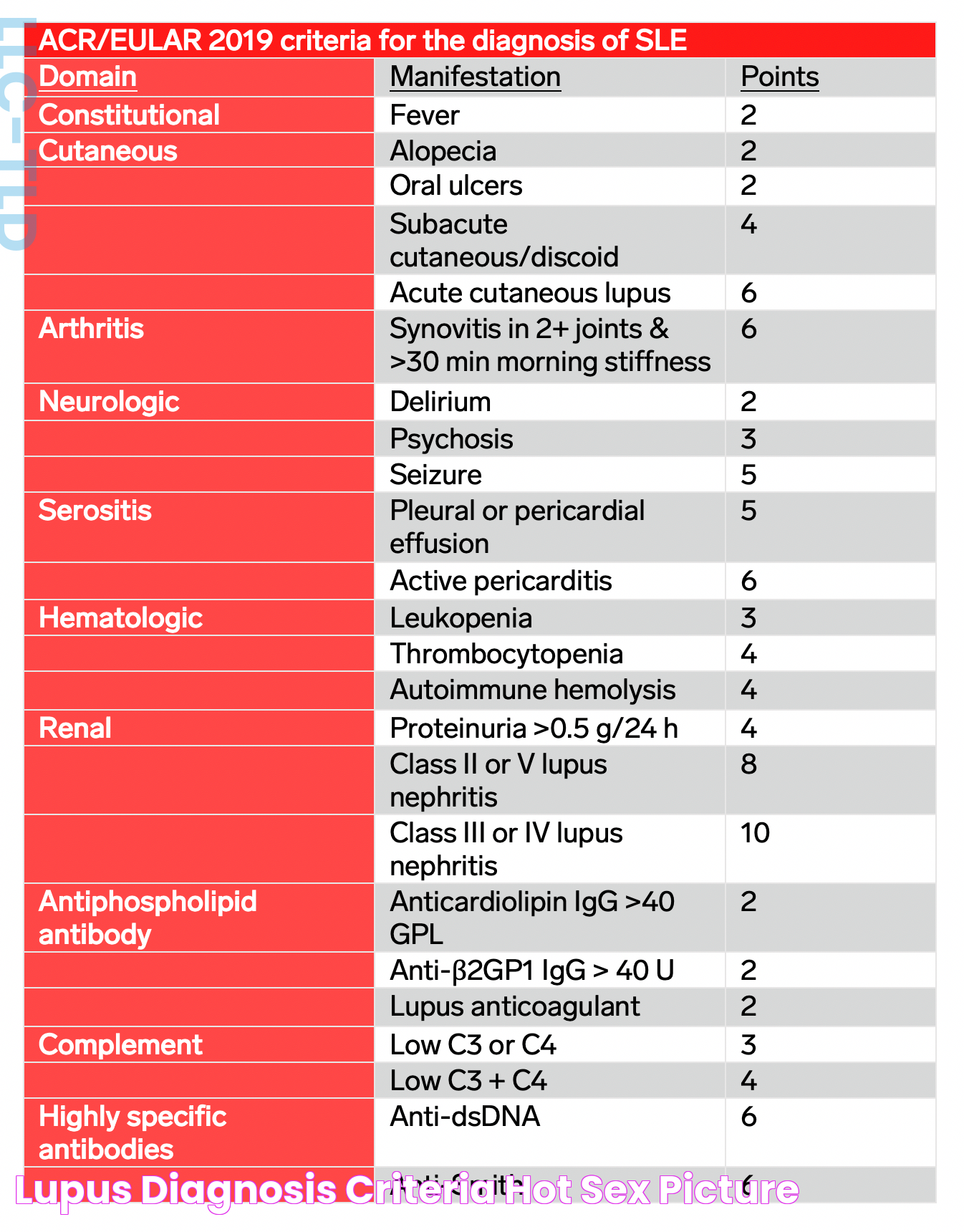
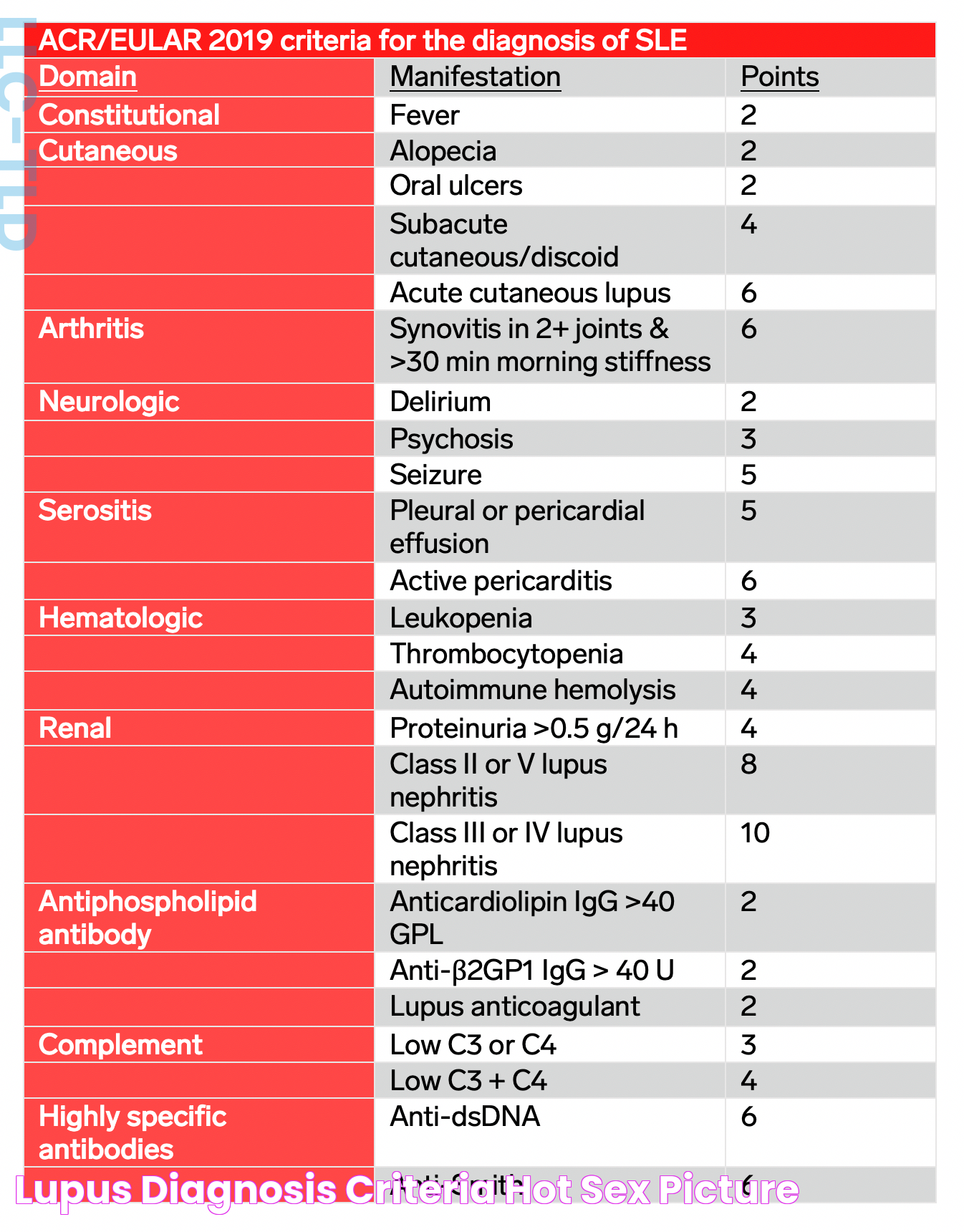
Diagnosing lupus involves meeting specific criteria established by medical organizations, which help standardize the diagnostic process and ensure accuracy. The most widely used criteria for lupus diagnosis are those developed by the American College of Rheumatology (ACR) and the Systemic Lupus International Collaborating Clinics (SLICC).
The ACR criteria, established in 1982 and updated in 1997, require the presence of at least four out of eleven specific clinical and laboratory findings for a lupus diagnosis. These criteria include:
- Malar rash (butterfly rash)
- Discoid rash
- Photosensitivity
- Oral or nasal ulcers
- Arthritis
- Pleuritis or pericarditis
- Renal disorder
- Neurological disorder
- Hematologic disorder
- Immunologic disorder
- Positive ANA test
The SLICC criteria, developed in 2012, require the presence of at least four criteria, with at least one clinical and one immunological criterion. Alternatively, a biopsy-proven lupus nephritis with a positive ANA or anti-DNA test is sufficient for diagnosis.
These criteria help healthcare providers systematically evaluate patients for lupus, ensuring a comprehensive assessment of symptoms and laboratory findings. It is important to note that meeting these criteria is not solely sufficient for diagnosis; clinical judgment and expertise are essential in interpreting the findings in the context of the patient's overall health.
The criteria for lupus diagnosis provide a structured approach to identifying the disease, guiding healthcare providers in making informed decisions about diagnosis and treatment. By adhering to these criteria, providers can ensure a consistent and accurate approach to diagnosing lupus across diverse patient populations.
Differential Diagnosis: Why it Matters?
Differential diagnosis is a critical aspect of the lupus diagnosis process, as it involves distinguishing lupus from other conditions with similar symptoms. This process is essential for ensuring an accurate diagnosis and avoiding potential misdiagnosis or inappropriate treatment.
Lupus shares symptoms with a variety of other diseases, including rheumatoid arthritis, fibromyalgia, multiple sclerosis, and chronic fatigue syndrome. These conditions can present with overlapping features such as joint pain, fatigue, and neurological symptoms, making it challenging to differentiate them from lupus.
To perform a differential diagnosis, healthcare providers will conduct a thorough assessment of the patient's clinical presentation, medical history, and laboratory test results. They may also consider other potential conditions and rule them out through targeted testing and evaluation.
The importance of differential diagnosis lies in its ability to ensure that patients receive the most appropriate and effective treatment for their specific condition. Misdiagnosing lupus or another condition can lead to ineffective treatment and potentially harmful outcomes.
By carefully evaluating and differentiating between potential diagnoses, healthcare providers can confidently identify lupus and tailor treatment plans to meet the unique needs of each patient. This approach enhances patient outcomes and supports the overall management of lupus and related conditions.
Impact of Delayed Lupus Diagnosis
Delayed lupus diagnosis can have significant consequences for patients, affecting their health outcomes and quality of life. Early and accurate diagnosis is crucial for initiating appropriate treatment and preventing long-term complications.
One of the primary impacts of delayed lupus diagnosis is the potential for disease progression and organ damage. Without timely intervention, lupus can cause irreversible damage to vital organs such as the kidneys, heart, and lungs, leading to severe complications and impaired function.
Additionally, delayed diagnosis can result in prolonged suffering and diminished quality of life due to unmanaged symptoms. Patients may experience chronic pain, fatigue, and emotional distress as they navigate the challenges of living with an undiagnosed condition.
The lack of a definitive diagnosis can also lead to frustration and uncertainty for patients, as they may undergo numerous tests and consultations without clear answers. This uncertainty can affect their mental and emotional well-being, contributing to anxiety or depression.
From a healthcare perspective, delayed diagnosis can lead to increased healthcare costs as patients undergo extensive testing and seek multiple opinions. Prompt and accurate diagnosis can help streamline the diagnostic process and reduce unnecessary expenses.
Recognizing the impact of delayed lupus diagnosis underscores the importance of early detection and intervention. Healthcare providers must remain vigilant in identifying potential lupus cases and employ a comprehensive approach to diagnosis and management to optimize patient outcomes.
Treatment Options After Lupus Diagnosis
Once a lupus diagnosis is confirmed, the focus shifts to developing a tailored treatment plan to manage symptoms and prevent complications. While there is no cure for lupus, various treatment options are available to help control the disease and improve quality of life.
Treatment plans for lupus are highly individualized and may include a combination of the following approaches:
- Medications: Depending on the severity and type of symptoms, healthcare providers may prescribe medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarials, immunosuppressants, or biologics.
- Lifestyle modifications: Patients are encouraged to adopt a healthy lifestyle, including a balanced diet, regular exercise, stress management, and adequate rest, to support overall well-being.
- Regular monitoring: Ongoing monitoring of symptoms and organ function is essential to assess treatment effectiveness and adjust the plan as needed.
- Patient education: Educating patients about their condition and treatment options empowers them to actively participate in their care and make informed decisions.
- Supportive therapies: Physical therapy, occupational therapy, and counseling may be recommended to address specific challenges and enhance quality of life.
The goal of lupus treatment is to minimize disease activity, manage symptoms, and prevent flare-ups. By working closely with healthcare providers, patients can develop a comprehensive treatment plan that addresses their unique needs and supports long-term health.
Effective management of lupus requires a collaborative approach between patients and healthcare providers, emphasizing open communication and shared decision-making. With the right treatment plan, patients can achieve better control of their condition and lead fulfilling lives.
Living with Lupus: Managing the Condition
Living with lupus presents unique challenges, as the disease can affect various aspects of daily life. However, with proper management and support, individuals with lupus can lead fulfilling and productive lives.
Managing lupus involves a proactive approach to health and well-being, focusing on symptom management, lifestyle modifications, and emotional support. Here are some key strategies for living well with lupus:
- Adhering to treatment plans: Consistently following prescribed medications and treatment regimens is essential for controlling disease activity and preventing flare-ups.
- Monitoring symptoms: Keeping track of symptoms and any changes can help identify patterns and triggers, allowing for timely intervention and adjustments in treatment.
- Maintaining a healthy lifestyle: A balanced diet, regular exercise, and sufficient rest can support overall health and enhance the body's ability to cope with lupus.
- Managing stress: Stress can exacerbate lupus symptoms, so incorporating stress-reduction techniques such as meditation, yoga, or deep breathing exercises can be beneficial.
- Building a support network: Connecting with family, friends, support groups, or mental health professionals can provide emotional support and encouragement.
Living with lupus requires adaptability and resilience, as patients may need to adjust their activities and lifestyle to accommodate the disease's demands. Open communication with healthcare providers and a willingness to explore new strategies can enhance the overall management of lupus.
Ultimately, individuals with lupus can thrive by taking an active role in their care, seeking support, and embracing a positive mindset. With the right resources and support, they can navigate the challenges of lupus and achieve a good quality of life.
Future Prospects in Lupus Diagnosis
Advancements in medical research and technology hold promise for improving lupus diagnosis and management. As our understanding of the disease continues to evolve, new diagnostic tools and treatments are on the horizon, offering hope for better outcomes for individuals with lupus.
Emerging areas of research in lupus diagnosis include:
- Biomarkers: Identifying specific biomarkers associated with lupus could lead to more accurate and earlier diagnosis, as well as personalized treatment approaches.
- Genetic research: Exploring the genetic factors that contribute to lupus may uncover new insights into its causes and potential targets for intervention.
- Advanced imaging techniques: Developing more precise imaging methods could enhance the detection and monitoring of lupus-related organ damage.
- Artificial intelligence (AI): Utilizing AI and machine learning algorithms to analyze complex data sets could improve diagnostic accuracy and predict disease progression.
These advancements have the potential to revolutionize the way lupus is diagnosed and managed, leading to more effective and tailored treatments for patients. As research continues, collaboration between scientists, healthcare providers, and patients will be crucial in driving progress and improving the quality of care for individuals with lupus.
The future of lupus diagnosis is bright, with ongoing research paving the way for innovative solutions and enhanced patient outcomes. By staying informed and engaged, patients and healthcare providers can embrace these advancements and work together to achieve a better understanding and management of lupus.
Frequently Asked Questions
What triggers lupus flare-ups?
Lupus flare-ups can be triggered by various factors, including stress, infections, sunlight exposure, certain medications, and hormonal changes. Identifying and managing these triggers can help reduce the frequency and severity of flare-ups.
Can lupus be cured?
Currently, there is no cure for lupus. However, with proper management and treatment, individuals with lupus can control symptoms, prevent complications, and lead fulfilling lives.
Is lupus hereditary?
While lupus is not directly inherited, genetic factors can contribute to an individual's susceptibility to the disease. Having a family member with lupus or another autoimmune disease may increase the risk.
Can men develop lupus?
Yes, men can develop lupus, although it is more common in women. Lupus affects approximately 10 times more women than men, but men with lupus may experience more severe symptoms and complications.
Are there any lifestyle changes that can help manage lupus?
Yes, adopting a healthy lifestyle can support lupus management. This includes maintaining a balanced diet, engaging in regular exercise, managing stress, getting adequate rest, and avoiding known triggers.
What is the life expectancy for someone with lupus?
With advances in treatment and management, the life expectancy for individuals with lupus has improved significantly. Many people with lupus can expect a normal lifespan, although the severity and complications of the disease can vary for each individual.
Conclusion
Accurately diagnosing lupus is a complex process that requires a thorough understanding of the disease's diverse symptoms and manifestations. Through a combination of medical history, physical examinations, laboratory tests, and imaging studies, healthcare providers can identify lupus and develop tailored treatment plans to manage the condition effectively.
While lupus remains a challenging disease to diagnose and treat, ongoing research and advancements in medical technology offer hope for improved diagnostic accuracy and patient outcomes. By staying informed and engaged in their care, individuals with lupus can navigate the complexities of the disease and achieve a better quality of life.
Ultimately, the journey to lupus diagnosis emphasizes the importance of a collaborative approach between patients and healthcare providers, fostering open communication and shared decision-making to optimize health and well-being.
Article Recommendations