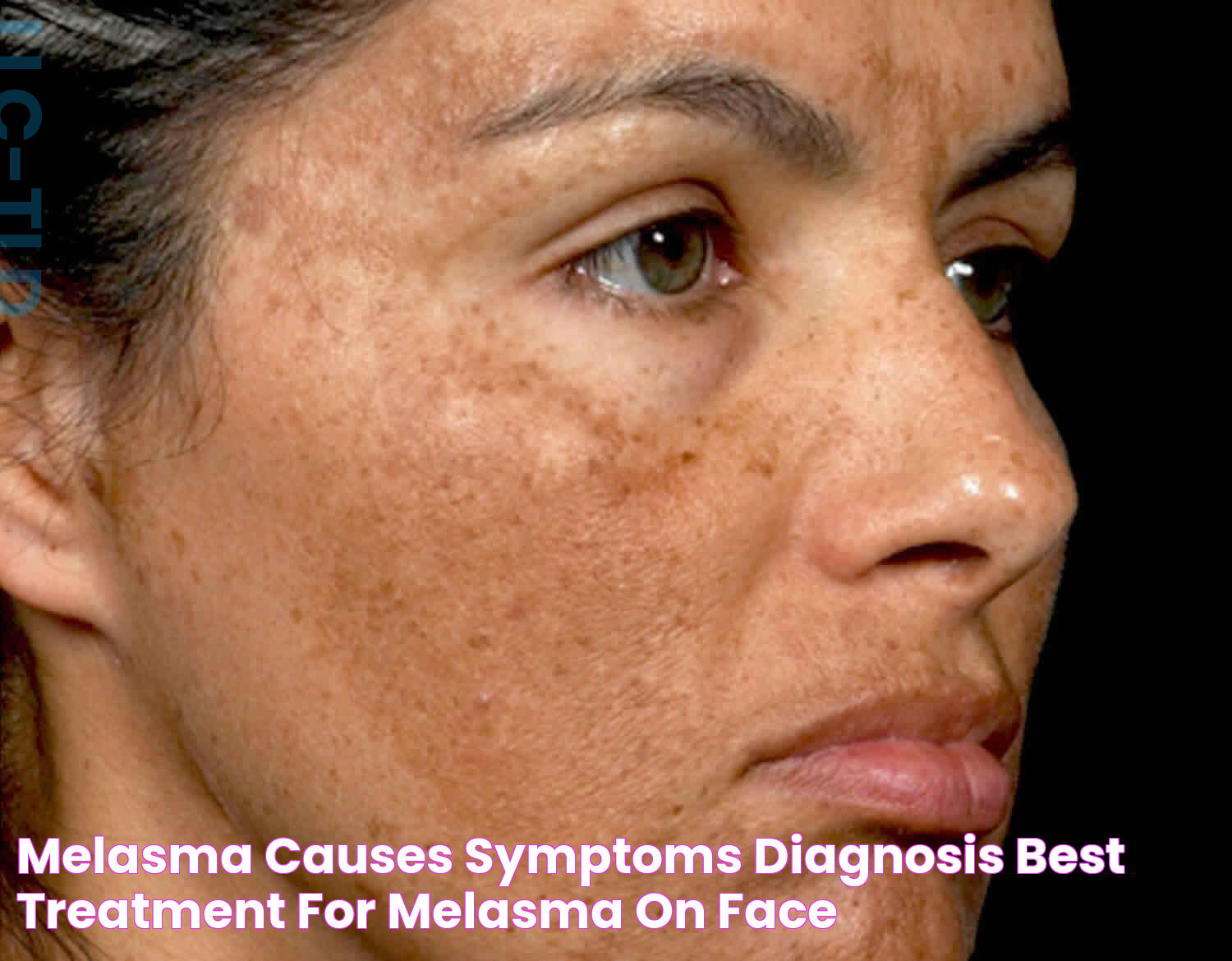
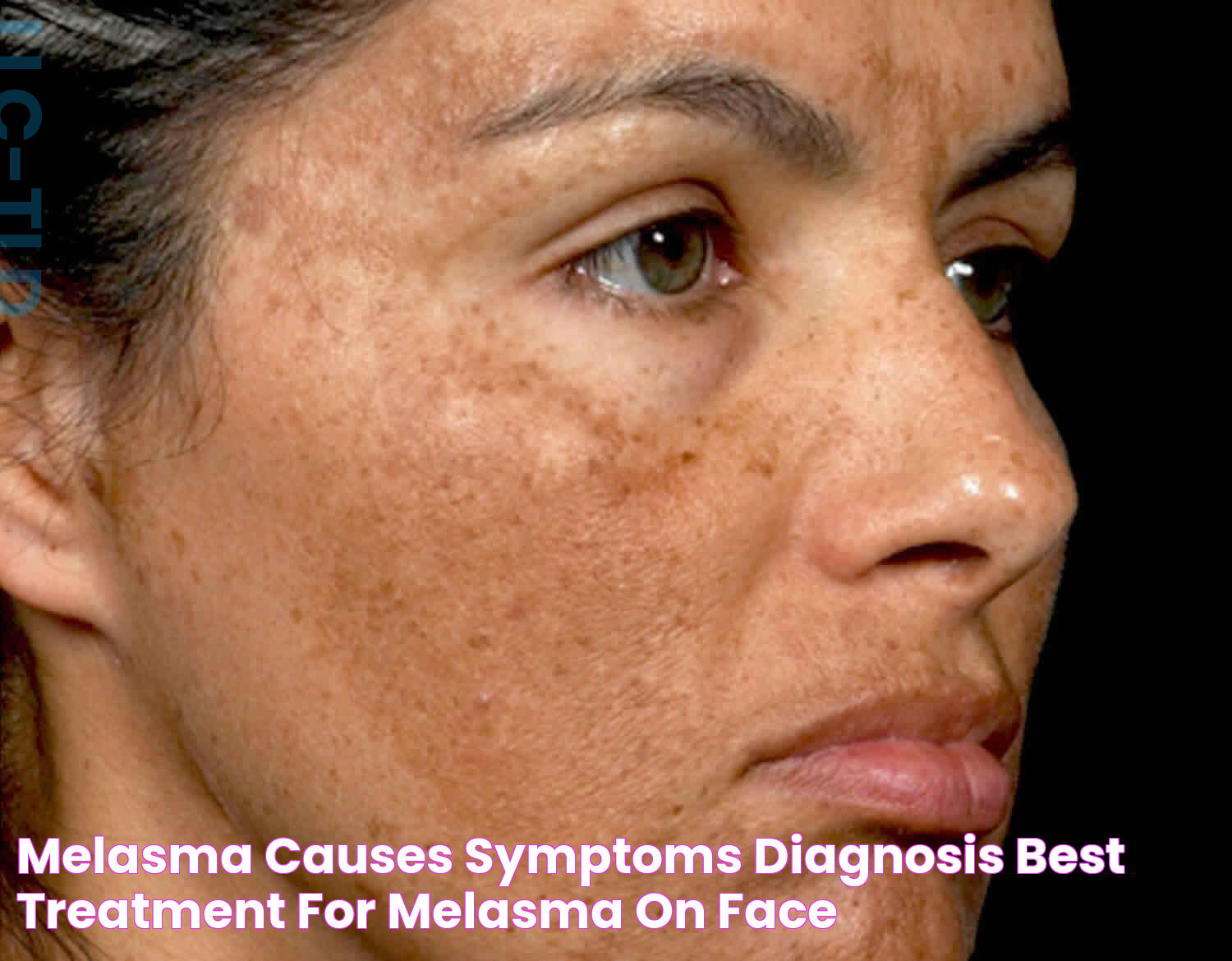
Melasma: A Comprehensive Guide To Understanding And Managing Skin Discoloration
Melasma is a common skin condition that manifests as brown or grayish patches on the skin, often appearing on the face. It can affect anyone, but is most prevalent in women, particularly those with darker skin tones. The condition is not harmful, but it can cause significant cosmetic concern and affect one's self-esteem. There is no singular cause for melasma, though it is generally believed to be triggered by hormonal changes, sun exposure, and genetic predisposition. Understanding melasma and its triggers is the first step towards effective management.
In recent years, there's been a growing interest in understanding "what is melasma" and how it can be effectively treated and managed. Despite its prevalence, many individuals remain unaware of the factors contributing to melasma and the available treatment options. This comprehensive guide aims to shed light on this skin condition, offering valuable insights into its causes, symptoms, and management strategies to help those affected make informed decisions.
The management of melasma often involves a multifaceted approach, including sun protection measures, topical treatments, and lifestyle modifications. With advancements in dermatological research and treatment options, individuals dealing with melasma can find hope in achieving clearer, more even-toned skin. This article will delve into the intricacies of melasma, providing you with a thorough understanding of this condition and guiding you towards effective solutions.
Read also:Remarkable History And Influence Of Diane Wildenstein
Table of Contents
- What is Melasma?
- Causes of Melasma
- Symptoms and Identification
- How is Melasma Diagnosed?
- Treatment Options for Melasma
- Topical Treatments for Melasma
- Lifestyle Changes and Prevention
- Does Diet Affect Melasma?
- Role of Sun Protection
- Can Melasma be Cured?
- Psychological Impact of Melasma
- Living with Melasma
- When to See a Dermatologist?
- Frequently Asked Questions
- Conclusion
What is Melasma?
Melasma is a chronic skin condition characterized by symmetrical, hyperpigmented patches, most commonly found on the face. These patches are usually darker than the surrounding skin and can appear on the cheeks, forehead, bridge of the nose, and upper lip. While melasma is not a medical concern, it can lead to emotional distress and affect one's quality of life.
Although the exact cause of melasma is not entirely understood, it is widely believed to be linked to hormonal changes, especially those related to pregnancy, birth control pills, and hormone replacement therapy. Sun exposure is also a significant factor, as UV rays can exacerbate the condition. Genetics may play a role, with a higher prevalence observed in individuals with a family history of melasma.
Melasma develops when the melanocytes, the cells responsible for producing pigment in the skin, become overactive. This overactivity results in the formation of dark patches. Women are more likely to develop melasma, with studies showing that it affects women nine times more frequently than men. Nonetheless, men can also experience this condition, although it tends to be less common.
Causes of Melasma
Understanding the causes of melasma is crucial for effective management. Several factors are believed to contribute to the development of melasma, including:
- Hormonal Changes: Hormonal fluctuations, especially during pregnancy or with the use of oral contraceptives, can trigger melasma. This is why melasma is often referred to as "the mask of pregnancy."
- Sun Exposure: Ultraviolet (UV) light from the sun stimulates melanocytes, increasing pigment production and worsening melasma.
- Genetics: A family history of melasma may increase the likelihood of developing the condition.
- Cosmetic Products: Certain skin care products, especially those that irritate the skin, may exacerbate melasma.
- Medical Conditions: Thyroid disorders and other medical conditions have been associated with melasma.
While these factors can contribute to melasma, the interplay between them can vary from person to person, making it a complex condition to understand and treat.
Symptoms and Identification
Identifying melasma involves recognizing its distinct appearance. The condition is characterized by:
Read also:Taryn Hanes An Inspiring Tale Of Talent And Tenacity
- Brown or Grayish Patches: The patches typically appear on the face, but can also be found on the neck and forearms.
- Symmetrical Patterns: Melasma usually presents in a symmetrical pattern on the face.
- Flat Patches: Unlike some other skin conditions, melasma patches are flat and do not cause any physical discomfort.
To accurately diagnose melasma, a dermatologist may use a Wood's lamp examination, which allows them to assess the depth of the pigmentation. In some cases, a skin biopsy may be performed to rule out other conditions.
How is Melasma Diagnosed?
Diagnosis of melasma is primarily based on the visual assessment of the affected skin. Dermatologists are trained to identify the characteristic patterns and colors associated with melasma. However, to confirm the diagnosis and assess the extent of pigmentation, additional diagnostic tools may be utilized:
- Wood's Lamp Examination: This involves the use of a special light that helps to determine the depth of melasma pigmentation, distinguishing between epidermal (superficial), dermal (deep), and mixed types.
- Skin Biopsy: In uncertain cases, a small skin sample may be taken for microscopic examination to rule out other conditions that cause skin discoloration.
Early and accurate diagnosis is essential in managing melasma, allowing for tailored treatment plans that address the specific needs of the individual.
Treatment Options for Melasma
Treating melasma can be challenging due to its tendency to recur and the influence of various factors on its development. A comprehensive approach, combining different treatments, often yields the best results. Treatment options include:
- Topical Treatments: These include hydroquinone, tretinoin, corticosteroids, and other agents that help lighten the skin.
- Chemical Peels: Mild chemical peels can help remove the outer layer of skin, reducing pigmentation.
- Laser and Light Therapies: Technologies such as fractional lasers and intense pulsed light (IPL) can target pigmentation and improve skin tone.
- Oral Medications: In some cases, oral medications such as tranexamic acid may be prescribed to help reduce pigmentation.
It's important to note that results can vary, and treatments may need to be adjusted based on individual responses. Regular follow-up with a dermatologist is crucial to monitor progress and make necessary modifications to the treatment plan.
Topical Treatments for Melasma
Topical treatments are often the first line of defense against melasma. These treatments aim to lighten the hyperpigmented areas and prevent further pigmentation. Common topical treatments include:
- Hydroquinone: A skin-lightening agent that reduces melanin production, hydroquinone is widely used in the treatment of melasma.
- Tretinoin: This topical retinoid helps increase skin cell turnover, promoting the shedding of pigmented skin cells.
- Corticosteroids: Often used in combination with other treatments, corticosteroids help reduce inflammation and improve treatment efficacy.
- Azelaic Acid: An alternative to hydroquinone, azelaic acid is effective in reducing pigmentation and is safe for long-term use.
For optimal results, these topical treatments should be used consistently and as prescribed by a dermatologist. Sun protection is also essential to prevent the recurrence of melasma during treatment.
Lifestyle Changes and Prevention
Preventing melasma is often easier than treating it once it has developed. Implementing lifestyle changes can significantly reduce the risk of melasma or prevent its recurrence. Key preventive measures include:
- Sun Protection: Regular use of broad-spectrum sunscreen with a high SPF is essential in protecting the skin from UV exposure.
- Protective Clothing: Wearing wide-brimmed hats and sunglasses can provide additional protection from the sun.
- Gentle Skin Care: Avoiding harsh skin care products and using gentle, non-irritating cleansers and moisturizers can help maintain skin health.
- Hormonal Management: For individuals who suspect hormonal triggers, discussing alternative contraceptive methods with a healthcare provider may be beneficial.
By incorporating these preventive measures into daily routines, individuals can minimize their risk of developing melasma and maintain healthier skin.
Does Diet Affect Melasma?
The role of diet in the management of melasma is still being explored, with some studies suggesting that certain dietary factors may influence skin health and pigmentation. While there is no specific diet for melasma, adopting a balanced and nutritious diet can support overall skin health. Considerations include:
- Antioxidant-Rich Foods: Consuming foods high in antioxidants, such as fruits and vegetables, can help protect the skin from oxidative stress.
- Hydration: Staying well-hydrated can support skin elasticity and overall health.
- Omega-3 Fatty Acids: Found in fish and flaxseeds, omega-3 fatty acids may have anti-inflammatory effects on the skin.
While diet alone may not cure melasma, maintaining a healthy diet can complement other treatment strategies and promote overall skin wellness.
Role of Sun Protection
Sun protection is a critical component in the management and prevention of melasma. UV radiation is a known trigger for melasma, and protecting the skin from the sun can prevent the worsening or recurrence of the condition. Key strategies include:
- Daily Sunscreen Use: Applying a broad-spectrum sunscreen with an SPF of 30 or higher every day, even on cloudy days, is essential.
- Reapplication: Sunscreen should be reapplied every two hours or more frequently if swimming or sweating.
- Timing and Shade: Limiting sun exposure during peak hours (10 a.m. to 4 p.m.) and seeking shade can further reduce UV exposure.
By diligently practicing sun protection, individuals with melasma can significantly improve the effectiveness of their treatment and reduce the risk of future pigmentation changes.
Can Melasma be Cured?
Melasma is a chronic condition that can be managed but not permanently cured. The aim of treatment is to reduce pigmentation and prevent recurrence. While some individuals may experience complete resolution of melasma, others may have persistent or recurrent patches.
Successful management of melasma requires a combination of treatments tailored to the individual's skin type, severity of the condition, and response to previous treatments. Ongoing sun protection and adherence to prescribed treatments are key to maintaining results and preventing flare-ups.
It's important for individuals with melasma to have realistic expectations and understand that while the condition can be managed effectively, it may require long-term maintenance and lifestyle adjustments.
Psychological Impact of Melasma
The visible nature of melasma can have a significant psychological impact on those affected, leading to feelings of self-consciousness and reduced self-esteem. The condition can affect social interactions and quality of life, particularly for individuals who are concerned about their appearance.
Addressing the psychological impact of melasma is an important aspect of treatment. Support from healthcare professionals, counseling, and support groups can help individuals cope with the emotional and psychological effects of the condition. Open communication with a dermatologist can also provide reassurance and guidance in managing melasma effectively.
Living with Melasma
Living with melasma involves adopting a proactive approach to skincare and lifestyle changes. Key strategies for managing melasma effectively include:
- Consistent Skincare Routine: Adhering to a skincare routine that includes sun protection and prescribed treatments is essential for managing melasma.
- Regular Dermatologist Visits: Routine check-ins with a dermatologist can help monitor progress and adjust treatments as needed.
- Emotional Support: Seeking emotional support from friends, family, or support groups can provide comfort and encouragement.
By taking a proactive approach and incorporating these strategies into daily life, individuals with melasma can manage the condition effectively and maintain healthy, radiant skin.
When to See a Dermatologist?
Consulting a dermatologist is recommended for individuals who suspect they have melasma or are experiencing persistent skin discoloration. A dermatologist can provide an accurate diagnosis, recommend appropriate treatments, and offer guidance on managing the condition. It's important to seek professional advice if:
- The skin discoloration is worsening or spreading.
- Over-the-counter treatments are ineffective.
- There is a desire to explore advanced treatment options such as lasers or oral medications.
Early intervention and expert guidance from a dermatologist can significantly improve the management of melasma and enhance treatment outcomes.
Frequently Asked Questions
What is melasma?
Melasma is a skin condition characterized by dark, discolored patches on the skin, commonly on the face. It is often associated with hormonal changes and sun exposure.
Is melasma permanent?
Melasma is a chronic condition that can be managed but not permanently cured. Treatment focuses on reducing pigmentation and preventing recurrence.
Can men develop melasma?
Yes, men can develop melasma, although it is more common in women. The condition presents similarly in both genders.
What is the best treatment for melasma?
The best treatment for melasma varies depending on the individual and may include topical treatments, chemical peels, or laser therapies. Consulting a dermatologist is recommended for personalized treatment plans.
Can stress cause melasma?
While stress is not a direct cause of melasma, it can exacerbate the condition by affecting hormonal balance and overall skin health.
How can I prevent melasma from recurring?
Prevention of melasma recurrence involves diligent sun protection, avoiding skin irritants, and following a consistent skincare routine as advised by a dermatologist.
Conclusion
Melasma is a complex skin condition that requires a comprehensive approach to manage effectively. By understanding the causes, identifying the symptoms, and implementing a tailored treatment plan, individuals can significantly improve their skin health and quality of life. Ongoing sun protection, lifestyle changes, and regular consultations with a dermatologist are critical components in the successful management of melasma. With the right approach, individuals can achieve clearer, more even-toned skin and regain confidence in their appearance.
For further reading and resources, consider visiting American Academy of Dermatology.
Article Recommendations